This model allows selected patients who are suited for remote care – such as those with conditions like cellulitis, respiratory issues, and heart failure – to receive high-quality hospital-standard treatment without needing to stay in a traditional ward setting.
Patients benefit greatly from this approach, as home-based care promotes faster recovery, reduces the disruption to their routines, and provides comfort for them and their families.
Since launching at the start of the year the adult Virtual Ward has transformed acute care delivery by offering comprehensive medical assessments, monitoring, and tailored treatment in patients’ own homes.
The programme has supported 262 patients so far, with positive feedback highlighting how this innovative service alleviates the strain on families and carers while enhancing the quality of recovery.
Peter Alexander, an 80-year-old resident of South Wootton, was recently admitted to the hospital in August with Necrotizing Otitis Externa – a rare but serious infection that affects the ear canal – and initially anticipated a three-month stay. However, thanks to the innovative Virtual Ward programme, Peter was able to return home after just three weeks to continue his recovery in the comfort of his own surroundings.
Peter shared, “It’s been such a blessing being able to recover at home. Initially, a nurse visited three time a day to administer IV antibiotics, but after a few weeks these were then given via a small pump over 24 hours meaning the nurse only had to visit once a day.
“I’m so grateful for the care I received through the Virtual Ward and cannot thank the team enough.”
His wife, Wendy, added, “It’s been an absolute godsend and has really helped Peter’s recovery. He’s been able to carry out normal activities at home, which would have been impossible in the hospital.”
Pippa Street, Chief Nurse at The QEH, said, “We know that patients recover quicker at home, where they can maintain their normal routines. Feedback from our Virtual Ward patients has been overwhelmingly positive; they appreciate the comfort of their own environment, which eases the pressure on families and caregivers.”
The adult Virtual Ward can accommodate up to 25 patients at a time, equipping them with a monitoring pack including a mobile phone and devices to track vital signs such as blood pressure and oxygen levels, which transmit real-time data to dedicated clinicians.
Patients remain under the care of a hospital consultant, supported by community and specialist teams from NCH&C. They receive personalised care, with regular virtual check-ins allowing clinicians to adjust medications, monitor health data, and collaborate with families to support a smooth recovery process.
This initiative not only supports faster recovery but also helps free up hospital capacity for patients who require inpatient care.
Simon Illingworth, Chief Operating Officer at QEH, commended the team’s efforts: “A huge well done to everyone involved. The entire team has made the Virtual Ward a success, leading to significant improvements in patient experience and care.”
Laura Clear, Deputy CEO and Director of Strategy & Transformation at NCH&C, said: “We’re delighted to be working closely with The QEH. This innovative service allows patients to receive hospital-level monitoring and treatment at home, preventing avoidable hospital admissions.”
The QEH also introduced a new paediatric Virtual Ward during the spring and so far more than 25 children have used the service.
This Virtual Ward, designed specifically for the needs of children, is a safe way of getting a patient home to a familiar setting with their family, where they can recover faster.
Tricia D’Orsi, Executive Director of Nursing at NHS Norfolk and Waveney Integrated Care Board (ICB), recently visited QEH’s paediatric Virtual Ward and praised its approach to remote care for children.
She said, “The paediatric Virtual Ward is an excellent example of how technology can be harnessed to provide high-quality, patient-centred care. I’m particularly impressed with the way it has been adapted for children and their families – it’s a model of modern healthcare that could pave the way for other hospitals to follow.”
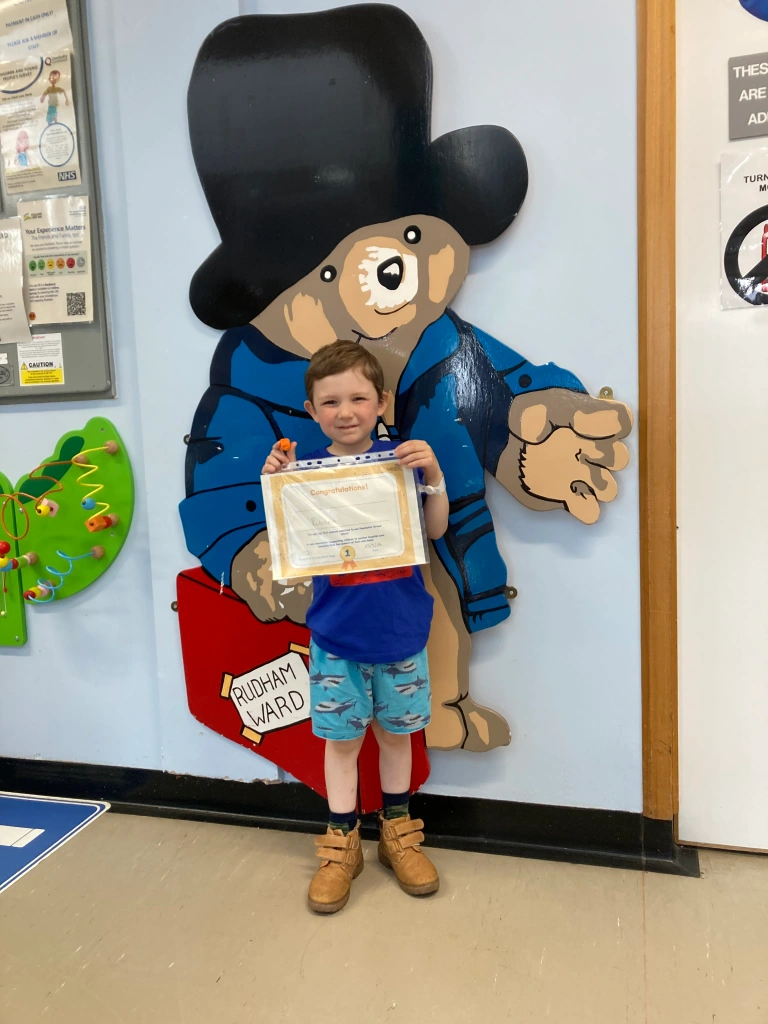
In May five-year-old Robson Dow, from Tilney St Lawrence, was the first patient to be admitted to the Trust’s children’s virtual ward.
His mum, Amy Withers, said: “It was great to be able to come home rather than stay in hospital. It meant Robson was able to be with both me and my partner and was much happier in his own surroundings.”
As QEH continues to innovate, the Virtual Ward stands as a powerful example of how modern healthcare solutions can enhance patient outcomes and experiences.